Vermont has its methadone clinics and (buprenorphine) suboxone doctors concentrated mostly in and around its metropolitan urban centers. With the recent rise in opioid addiction problems across the United States, more medical providers are preparing themselves to assist people suffering with moderate to severe opioid dependency. While some individuals are able to detox successfully from opioids under supervised care, many discover that medication-assisted treatment is necessary to help them either avoid painful opioid withdrawal or to facilitate their journey into long term recovery. Methadone and (buprenorphine) suboxone are the two most popular & effective medication-assisted therapies available for opiate addicted persons. Both medications are FDA-approved, SAMHSA endorsed, and have been successfully utilized in treating opioid addiction for more than a decade. With methadone in particular, its success profile dates back to over 40 years in the United States. Federal Rules For Methadone Access Are Changing
The Biden administration has created new federal rules for methadone treatment designed to widen access for more patients. In particular, the requirement of one year of active opioid addiction is being reduced to just 6 months of opioid addiction in order to become eligible to receive methadone. There are about 2000 federally-approved opioid treatment programs (OTP) in the United States. Many thousands of patients are receiving life saving services from these clinics. Since COVID, many OTP clinics have made take home medication more accessible to those in early phases of treatment. With illegal opiates still flooding the country, increasing access to opioid treatment and medication is easily justified. The question remains as to how local law enforcement can ultimately stem the flow of drugs into the community, as well as how youth can be educated to avoid risking first drug use.
Posted in Buprenorphine, Harm Reduction, Methadone, Methadone Clinics, Methadone Take Home, Opioid Treatment, Prescription Drugs, Suboxone
Tagged buprenorphine, methadone
Comments Off on Federal Rules For Methadone Access Are Changing
How Bad Is Opioid Withdrawal
In the video, Sarah explains how opioid withdrawal can become so severe with diarrhea and vomiting that individuals can die from extensive dehydration. As physicial dependency progresses, the brain becomes increasingly imbalanced and unable to function without the presence of opioids. When opioid withdrawal commences (usually 8-12 hours after last use), it becomes increasingly unbearable as the body is flushed with stress hormones. The withdrawal discomfort builds in intensity over days, and can last up to a week or more. For many, this withdrawal process feels akin to a severe case of the flu, but then potentially reaches levels of sickness even far beyond that. In the video, Sarah goes on to discuss the benefits of methadone and buprenorphine in reducing severe withdrawal symptoms and in helping patients to ultimately not die from overdose. She also illuminates on how rational decision-making is so extremely difficult when struggling against the intense pain of opioid withdrawal. Please check this video out, and share it with anyone you believe can benefit from its message.
Posted in Buprenorphine, Medication Assisted Treatment, Methadone, Methadone Clinics, Opiate Withdrawal, Opioid Treatment, Pain Management, Prescription Drugs, Suboxone
Tagged Fentanyl
Comments Off on How Bad Is Opioid Withdrawal
Helping Skeptics Understand Methadone
Sadly, addiction leads people to behave in ways that make no sense to their family, friends, and co-workers. Therein lies an important part of the problem. Family feel confused, angry, and fearful as their loved one tumbles down the hill of active addiction. When it comes to something as perplexing as drug addiction, grasping for answers is an understandable reflex for family and friends. What family often don’t comprehend is the power of physical dependency to opioids and the severe sickness that results from opioid withdrawal. Family and others incorrectly assume that mere “choice” is all that’s needed to overcome the addiction. When the addict fails to remain drug free, harsh judgment by others usually follows. Halting withdrawal sickness is a paramount step for an opioid addicted person. This cannot be overstated. As long as a person is suffering from severe opioid withdrawal, their ability to think and “choose” logically is greatly impaired. Statistically, individuals who utilize medication-assisted treatment (like methadone) are far more likely to avoid incarceration, a continued downward spiral, or death by overdose. Medication assistance successfully removes debilitating withdrawal sickness so that the addicted person can experience greater clarity of thought and the ability to make more sound decisions that lead to improved quality of life. If you are a skeptic about methadone or suboxone, you may think “they’re just trading one drug for another”. This is not true. People, once therapeutically stabilized on methadone or suboxone, do not get high from the medication. Health generally improves, and the person is able to function much better on the job and at home. This brings hope. It offers a new opportunity for further recovery. When you care about a person’s survival, one more chance to help them can be quite valuable. Don’t let judgment or excessive skepticism get in the way. Medication-assistance in opioid recovery is effective for many people, and it has been the life saving next step that some never got the chance to take.
Posted in Methadone, Methadone Benefits, Methadone Clinics, Recovery, Suboxone
Tagged methadone benefits
Comments Off on Helping Skeptics Understand Methadone
Methadone Treatment in Oregon
This article, in the Hillsboro News-Times, features the recent approval by Washington County commissioners to add a new methadone clinic in Hillsboro, Oregon. Acadia Healthcare is aiming to establish the new methadone clinic in Hillsboro in order to better serve the local community. Acadia already operate a mobile unit in the general area as well as a comprehensive treatment center (CTC) in nearby Tigard located about 20 miles away. The commissioners voted 5-0 to approve the proposed site which will be on the local bus route thereby providing improved access. The article mentions that Oregon presently has 17 operational methadone clinics serving the state, where fentanyl, opiates, and other substances are causing a grave overdose crisis. Having local opioid treatment available is a critically important step in saving lives and providing hope to patients and families. Methadone has been proven to decrease opioid use, reduce relapse risks & overdose deaths, as well as increase employment and overall health. Clinics offering medication-assisted treatment (MAT), like methadone and buprenorphine, are forging a new path to safety for those people once stuck in active addiction.
Posted in Acadia Healthcare, Addiction Treatment, Buprenorphine, Methadone, Methadone Clinics, Oregon Methadone Clinics, Suboxone
Tagged Acadia, methadone treatment, Oregon
Comments Off on Methadone Treatment in Oregon
Remote Observation of Methadone Dosing
The project is evaluating this new modified approach that falls somewhere between in-person daily dosing and unsupervised take home dosing. This new approach is currently being referred to as Video DOT (video direct observation therapy) and has been successfully implemented with other health issues including hepatitis C, asthma, and diabetes. While this experiment seems appealing at first glance, it does raise legitimate questions about the ability to insure proper safety protocols with the provision of methadone medication to new patients. The project may possibly demonstrate the usefulness of Video DOT methadone dosing. But assuming this new approach one day becomes common practice, it will be important that physicians or clinics have in place a procedure for quickly reclaiming methadone doses that are not ingested on schedule. Imagine a new patient receives 7 take home doses of methadone, but then only sends in the required video of their medication use on day one. At what point does the prescribing clinic intervene, and how will the unaccounted for doses be retrieved? Approved Opioid Treatment Programs currently have “callback” procedures in which stable patients are randomly selected to return to their home clinic with their unused take home doses. This allows the clinic medical staff to perform a medication count, and it acts as a safeguard to insure patients are taking their medication as prescribed. Patients who have earned take home privileges through months of treatment progress are less inclined to divert or misuse methadone than someone who just started treatment. New patients must be inducted gradually on a stabilizing dose of methadone. And time is typically needed to help these patients adjust to methadone while eliminating use of all other illicit substances. This is where the benefit of a structured treatment program is most relevant. OTP’s provide extremely valuable life management skills training in conjunction with medication therapy. It remains to be seen if “easy access” to methadone is truly an advancement in care, or a step backwards in accountability & safety for patients and the public.
Posted in Medication Assisted Treatment, Methadone, Methadone Clinics, Methadone Programs, Suboxone, Suboxone Clinics
Tagged Remote Methadone Dosing
Comments Off on Remote Observation of Methadone Dosing
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 The synthetic opioid, fentanyl, has led to an increase in overdose deaths in recent years. As many as 112,000 in the last year
The synthetic opioid, fentanyl, has led to an increase in overdose deaths in recent years. As many as 112,000 in the last year  There is an
There is an  When it comes to addiction, reactions and opinions are often intense. Addiction is a devastating illness that can rapidly derail a person’s life, and seriously impact the lives of those around them.
When it comes to addiction, reactions and opinions are often intense. Addiction is a devastating illness that can rapidly derail a person’s life, and seriously impact the lives of those around them. Like most states, Oregon is in need of quality treatment options for opioid-addicted individuals who are ready for recovery.
Like most states, Oregon is in need of quality treatment options for opioid-addicted individuals who are ready for recovery. 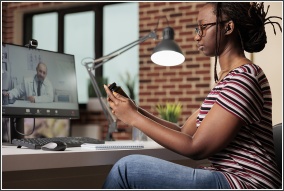 There’s a new spin being proposed on the dispensing of methadone to Opioid Use Disorder (OUD) patients. A federally-funded
There’s a new spin being proposed on the dispensing of methadone to Opioid Use Disorder (OUD) patients. A federally-funded